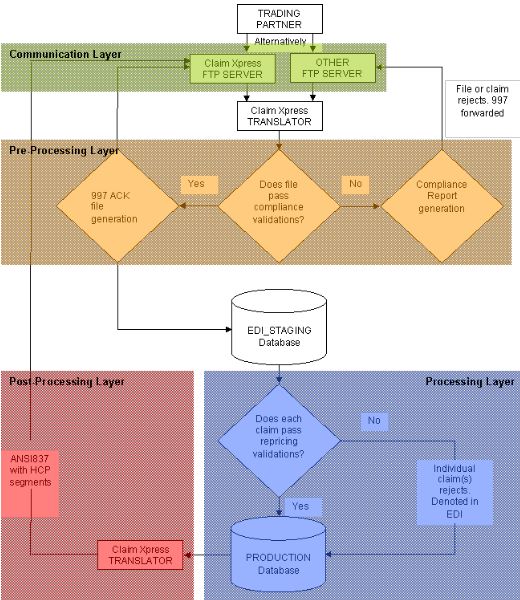
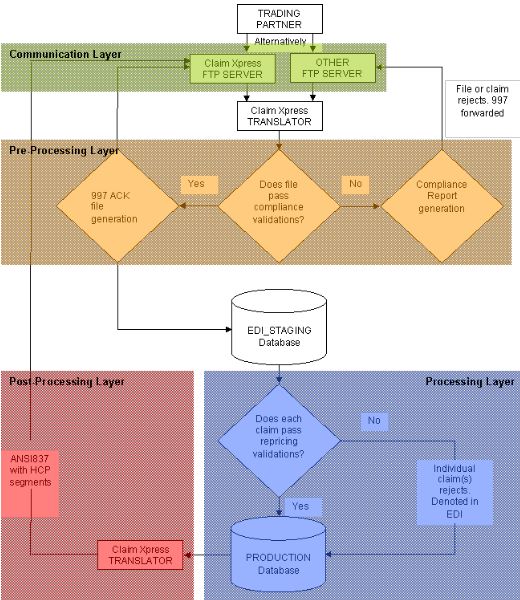
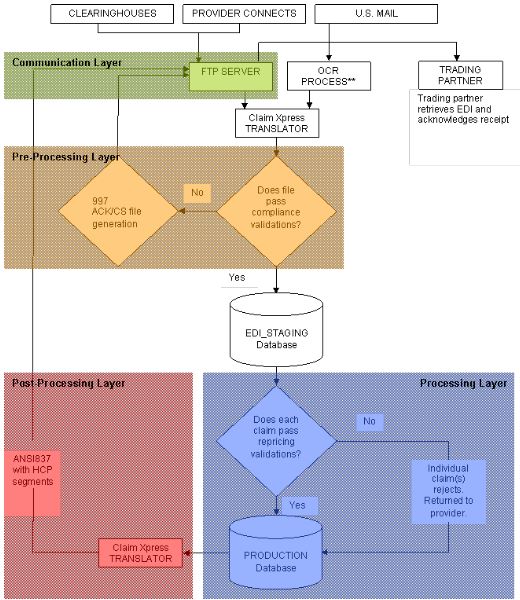
Direct Connect Model (figure 1.1)
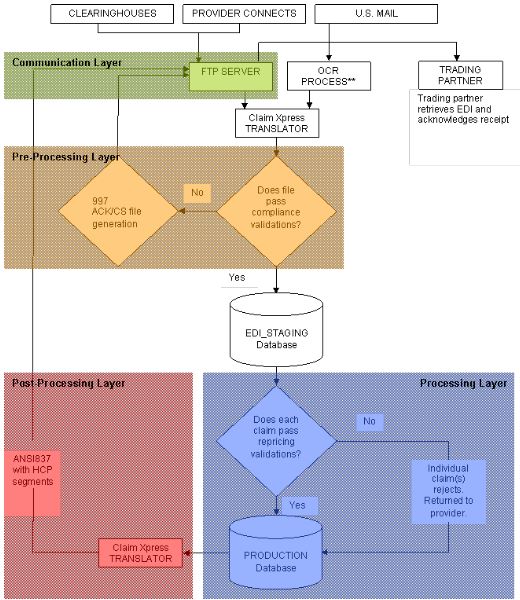
Traditional Model (figure 1.2)
The MCO Pro system handles the following ANSI standards:
MCO Pro can automatically retrieve EDI claim files from any number of sources and parse these claim transactions into the MCO Pro system. The system supports two models of EDI exchange. Figures 1.1 and 1.2 flowchart these models:
In addition the MCO Pro system has the following capabilities in regards to EDI:
As claims are parsed into the system, MCO Pro compares inbound Insured’s and Patient’s to the eligibility subsystem. If a “hit” is found, the system then compares inbound billing and rendering providers against the provider file. If a “hit” is found, the claim auto-prices without any user intervention. Historically the system auto-prices more than 40% of claim transactions in the first 3 months of use. As eligibility and provider billing tendencies are recorded this percentage continues to rise as more and more claim transactions pass through the system.
From claim research screens, users can identify the source of the claim (clearinghouse, direct connect, scanned paper), the file the claim was transmitted in, the date the claim was sent out, the file name the claim was transmitted in, acknowledgements and can view either the inbound or outbound EDI. In addition the claim image can be retrieved along with the repricing (remittance advice) cover sheet.
By utilizing technologies developed by a ClaimEDIx strategic partner, your inbound paper claims can be converted to electronic (EDI) transactions. This process greatly reduces claim handling costs and allows much of your paper volume to auto-price.
In conjunction with optical character recognition, the MCO Pro system builds an image library tying claims residing in the database with the image(s) of the claim after scanning.
Want more information about ClaimEDIx solutions?
Reach out to us; we would love to help you.